May 28, 2015
Preparing the Ocular Surface for Cataract Surgery
published on May 28, 2015 by
The condition of a patient’s ocular surface prior to cataract surgery, particularly refractive cataract surgery, can greatly impact the outcome. This is especially true for patients with dry eye and/or mild or severe epithelial basement membrane dystrophy (EBMD). Both of these conditions are so prevalent, they can be easy to overlook. I was taught in residency, 10% of the population, but if you look at the studies, it’s widely variable. Some studies are upwards of 30 to 40% of the population.
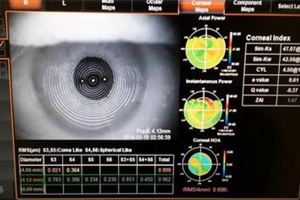
As we all know, the cornea can gradually change shape over time. However, with EBMD, the corneal power is typically irregular and changing unpredictably. This challenging patient population has taught me a few lessons along the way that has really impacted my approach to ocular surface rehabilitation prior to cataract surgery.
Consider these questions:
- How do you handle EBMD patients who need cataract extraction?
- Are you shying away from refractive cataract surgery and premium IOL’s in these patients due to concerns about outcomes?
- Are you getting post-operative refractive surprises?
- Does your enhancement method change depending on the presence of EBMD?
In my opinion, the diagnosis and management of EBMD is vitally important prior to cataract surgery. I was told early on in my career that anything I diagnose and discuss with a patient before surgery is their problem; anything I tell them after surgery becomes my problem to fix. As we know, these patients present significant challenges in getting accurate biometric measurements. The presence of EBMD in the central 3-5mm creates chaos when trying to obtain accurate keratometry readings. In my opinion, there is no better patient population to consider a prophylactic superficial keratectomy than those with EBMD and cataracts. By removing the irregularities, you have the opportunity to reset the corneal curvature back to its foundational shape. When implanting a lens, we are providing a permanent refractive change. Taking off the epithelium and letting it heal gives me much more confidence in my biometry and choice of IOL.
This ocular surface disease, EBMD and cataract patient population is potentially at risk for delayed re-epithelialization. However, I have found that using cryopreserved amniotic tissue (Prokera®) at the time of superficial keratectomy, I have much less to worry about. It accelerates healing and restores the ocular surface to a pristine state quickly. We find that this therapy rejuvenates the ocular surface to allow us to get accurate biometry in as little as four weeks.
The biological elements of cryopreserved amniotic tissue decrease inflammation and scarring, allowing for faster healing without haze. This is particularly beneficial with a superficial keratectomy; traditional treatments such as a bandage contact lens don’t have the biological healing elements found in cryopreserved amniotic tissue. This is important for many patients with active and busy lives who don’t want to wait long to have surgery. And, cryopreserved amniotic tissue delivers better results; patients have pristine corneas with less haze, enabling me to talk to them about a premium IOL option that previously I would not have been comfortable doing.
By addressing pre-existing ocular surface disease, we can improve patient satisfaction and outcomes in cataract surgery. For more information, download “Accelerate Healing of the Ocular Surface Prior to Cataract and Refractive Surgery”.
