March 29, 2016
Reducing Pterygium Recurrence: Improve Surgical Outcomes with This Time-Saving Technique
published on March 29, 2016 by
After working my way through the painstaking troubles of some of the traditional approaches to pterygium surgery, I thought there must be a better way. Through time, I developed a new approach that I call the Tissue Tuck Technique. This technique fulfills all the criteria that, in my mind, define successful pterygium surgery. It’s efficient, reproducible, and not difficult. It has an excellent cosmetic result. And, most importantly, it has a low recurrence rate. After using this new technique in more than 700 cases, my recurrence rate is less than 1%.
A Key Ingredient
Crucial to the development of the technique and its success is AmnioGraft® cryopreserved amniotic membrane tissue. Because it’s easy to manipulate, I can place, reposition, and tuck it exactly where it’s needed. In contrast, amniotic tissue preserved by dehydration isn’t as resilient, nor does it retain the anti-fibrinogenic, anti-inflammatory, anti-scarring, or anti-angiogenic properties of fresh amniotic membrane as AmnioGraft does. These properties reduce pain, expedite recovery, and lead to a superior cosmetic outcome.
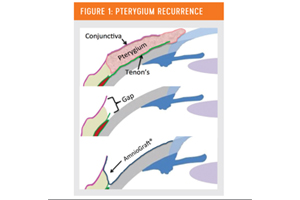
As we know, a pterygium is fibrovascular tissue caused by solar elastosis of the substantia propria, and it originates and grows from the space between Tenon’s and normal conjunctiva. This is the area we refer to as “the gap.” The Tissue Tuck Technique is designed to effectively seal the gap because it’s also the origination point of recurrences (Figure 1).
A New Procedure
Key steps in the procedure are:
- Resect the head and body of the pterygium, leaving bare sclera and an intact muscle sheath.
- Create a 2-mm to 3-mm perimeter of normal conjunctiva by pulling Tenon’s and remaining fibrovascular tissue anteriorly from under the conjunctiva and resecting it. (Tenon’s has a natural tendency to recess itself, which helps to produce the desired clear perimeter of conjunctiva.)
- Cauterize the band of Tenon’s, fibrovascular tissue, and prolapsed orbital fat in the posterior and nasal aspects of the gap between Tenon’s and the resected conjunctival rim, avoiding the muscle belly, overlying conjunctival rim, or overly aggressive cauterization of the scleral bed.
- Bring the AmnioGraft into the field and trim to the general shape of the exposed bed, but oversizing by 2 mm to 3 mm to allow adequate tissue for tucking and re-creation of the semi-lunar fold.
- Slide the graft over the bed, coat the stromal side with glue, and place it overlapping the edge of the conjunctival rim and intended semi-lunar fold.
- Use curved tying forceps to tuck the tissue under the conjunctival rim and deep into the gap along the entire new semi-lunar fold.
- Use the forceps to pinch the edge of conjunctival rim to the folded and tucked tissue to seal and create a wide margin of contact.
- Squeegee away any excess glue with an anterior motion so glue isn’t pushed into the gap.
- Trim any excess AmnioGraft and insert a bandage contact lens to protect the anterior edge of tissue.
I use Mitomycin C only in cases of severe or recurred pterygia, or when a patient’s ethnicity or occupation would make him or her prone to recurrence.
On average, I can perform the Tissue Tuck Technique in 10 to 12 minutes. It’s sutureless, which saves both time and cost, and eliminates a potential source of inflammation. Recovery to the point of fair cosmesis is 1 to 2 weeks.
In the meantime, patients have little or no discomfort. My postoperative regimen used to include NSAIDs and oral painkillers, but with this technique, I’ve taken both of those away. Patients do very well with only a topical steroid and antibiotic.
Neel Desai, MD is a cataract and refractive surgeon at The Eye Institute of West Florida, in Largo.
