A 45 year-old gentleman was referred to me for HSV keratitis. Over the course of a six to eight year period, the patient had at least 10 recurrent stromal herpetic episodes that he could recall. He had been a police officer for over 15 years, and because of his vision, he didn’t feel safe at nighttime and in dim lit conditions. Due to his condition, he was at risk of having to resort to a desk job permanently or possibly leaving his career altogether.
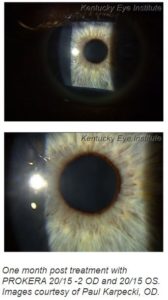
When I first examined the patient, his vision was 20/25-2 OD, 20/15 OS, but in these cases it’s about the quality of vision, which is most noticeable at night. He felt like the deterioration in his right eye was also starting to affect his other eye. He had grade 2 conjunctival injection and dense but anterior stromal opacities. There was no corneal staining and the anterior chamber was deep and quiet. He was on oral Valtrex for prophylaxis to prevent further recurrences. Since the original stromal lesions had gone back many years, I knew this would be a difficult case to treat (see image prior to treatment).
I explained to the patient that I’ve had great success with cryopreserved amniotic membrane (Prokera®) however, I hadn’t used it to treat scarring and haze that had been occurring for so long. But because it was superficial and wasn’t deep stromal, I felt we had a good chance of improving his condition, albeit this being somewhat relative as it may just be slightly noticeable. To set his expectations, I gave him these odds: about a 70 percent chance we could improve his vision, a 25 percent chance he wouldn’t notice a difference, a 4 percent chance we would clear the eye completely, and a 1 percent chance it would get worse. I wanted to be realistic and didn’t want him having the expectation his cornea would be completely clear after treatment.
I went over what we were going to do to place the Prokera Slim, did the insertion, and taped his eyelids, which I prefer to do as I feel it helps patients better tolerate treatment. And although I haven’t formally studied this, I feel that I get longer duration of the Prokera membrane when I have the eyes closed the entire time. I recommended he continue the oral Valtrex (500mg QD) and if he felt any discomfort, pain or scratching, to let me know, otherwise we would see him in five days for removal. He expressed only minor discomfort during that time, and when he came back to have Prokera removed, it was pretty much dissolved so we took it out. There was some improvement, which to my delight the patient noticed as is not always the case on day one. I told him to continue the Valtrex and we would see him back in a month to see how he is doing.
When the patient returned a month later, his vision was 20/15 OD and 20/15 OS and the haze and scarring was hardly noticeable (see images post treatment). His vision was comparable to his other eye and needless to say he was ecstatic. As a result he was able to safely return to his regular duties as a police officer on the streets knowing he, his partner and the public were safe. After three months, I saw him again and his cornea was still clear just like as in the original image.
It’s been about a year now, and so far the patient hasn’t returned with any episodes. I did educate him that there is about a 50 percent chance of recurrence with stromal keratitis due to it being systemic, but by using the oral prophylactic anti-virals it does reduce the risk. And according to the Herpetic Eye Disease (HEDS) study, the severity is decreased by 67 percent, so it’s a good idea to maintain that course.