Neurotrophic Keratitis
Are you checking corneal sensitivity on your SPK patients?
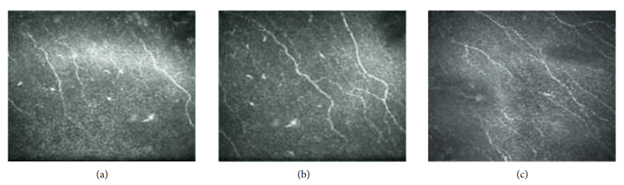
According to the Mackie classification, stage 1 Neurotrophic Keratitis (NK) begins as early as Punctate Epithelial Keratitis (PEK).12
Discovering and Treating the Underlying Cause
Neurotrophic Keratitis (NK) is a corneal degenerative disease characterized by a reduction of corneal sensitivity.1 In NK, corneal innervation by the trigeminal nerve is impaired.1
This can lead to corneal epithelial breakdown, impairment of healing, and development of corneal ulceration, melting, and perforation.2 NK abolishes both tearing and blinking reflexes, thus causing the most severe forms of Dry Eye Disease (DED).3
Did you know the American Academy of Ophthalmology has recognized Prokera® as a stage 1 treatment option1?
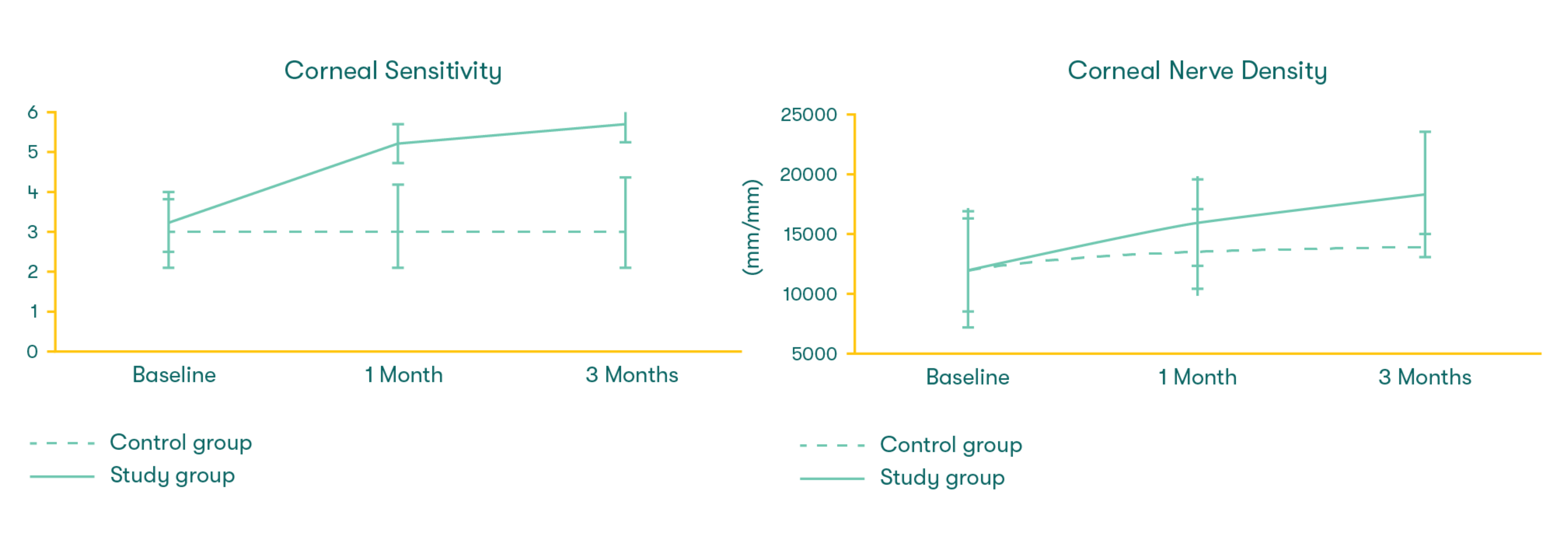
Prokera cryopreserved amniotic membrane helps regenerate corneal nerves as it accelerates the recovery of corneal surface health.7 Prokera has been shown to significantly reduce the signs and symptoms of DED as stated in Thomas John’s study.7 Prokera has also been used successfully to treat corneal defects and ulcers caused by NK, which were non-responsive to prior treatment as reported in other prospective studies.9-11

How can I test for Neurotrophic Keratitis?
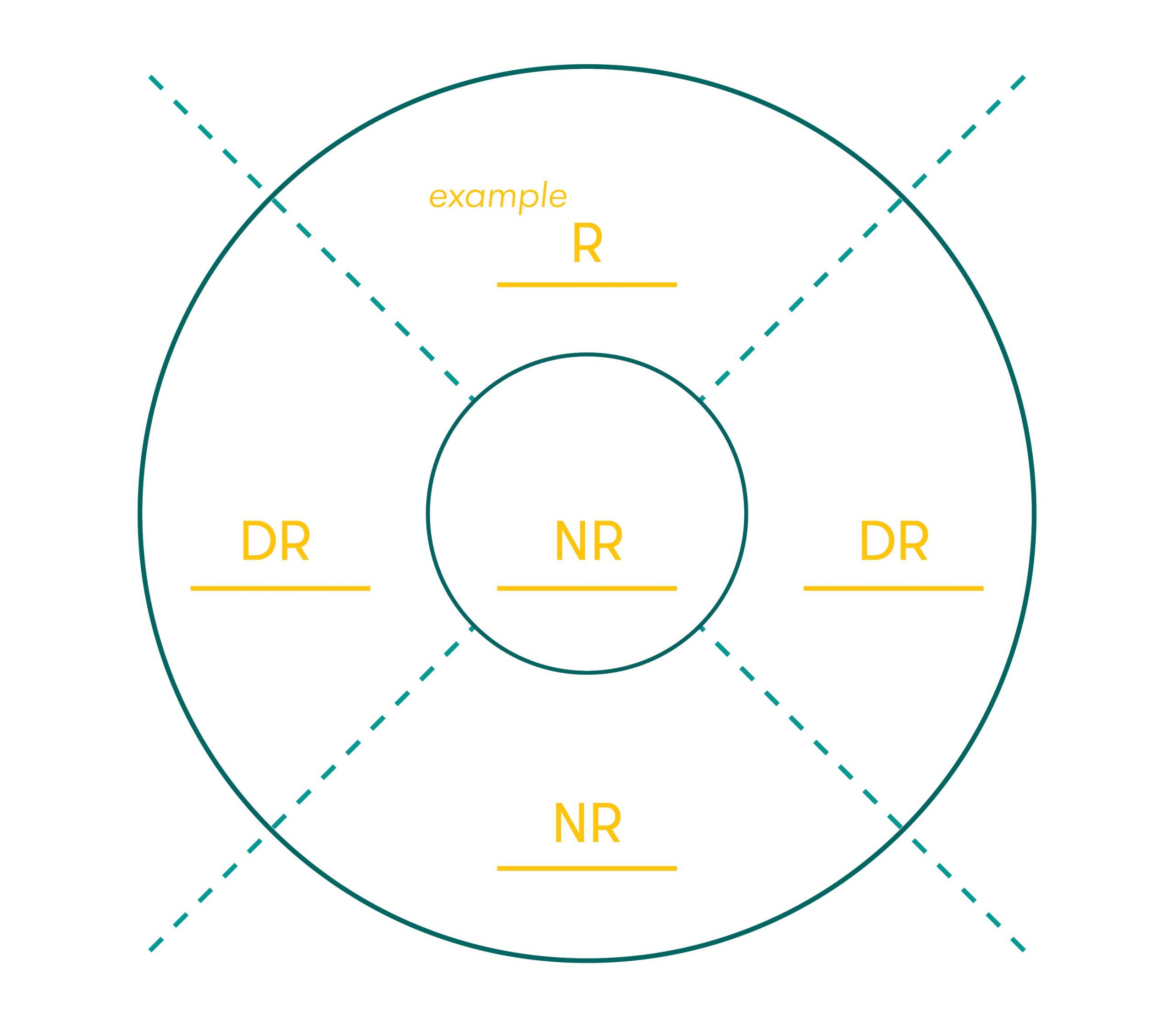
Assessment of corneal sensitivity is essential to confirm the diagnosis of NK and to assess the severity of corneal nerve impairment. Corneal sensitivity can be measured qualitatively by touching the central and peripheral cornea with a cotton thread or quantitatively using a corneal aesthesiometer.8 When the cotton thread gently touches the cornea, patients with a normal cornea show a blink reaction and can describe the sensation of touch, while patients with loss of corneal sensitivity do not react.
Label the chart with level of sensation using the Sensation Key.
Sensation Key
R – Responsive (Normal)
DR – Delayed Response (Reduced)
NR – Non-responsive (Absent)