Dry Eye Syndrome, Exposure Keratopathy
Dry Eye Syndrome, Exposure Keratopathy
Dry Eye Syndrome, Exposure Keratopathy
Peter Andrews, MD, is a board-certified, fellowship-trained cornea, external disease, and refractive surgery specialist at the Eye Care Center of Northern Colorado. He graduated from medical school at the Wake Forest University School of Medicine and completed his ophthalmology residency and fellowship training at the University of Florida. He is a trained cornea specialist performing procedures such as LASIK, PRK, ICLs, INTACS for keratoconus, corneal transplants, DSAEK and DMEK techniques, and cataract surgery. He is a speaker for BIO‑TISSUE® and can be reached at (303) 772-3300.

PETER ANDREWS, MD – LONGMONT, CO
Overview
Dry eye syndrome (DES) is characterized by tear film instability and ocular surface inflammation, which in turn causes cell damage, resulting in a self-perpetuating cycle of deterioration.6 Several proinflammatory cytokines including interleukin 1 (IL-1), IL-6, IL-8, transforming growth factor-beta (TGF-ß), and tumor necrosis factor (TNF-α) are upregulated in DES. Elevated levels of tissue-degrading enzymes such as matrix metalloproteinases (MMPs) are also noted.7 DES may be complicated by sterile or infectious corneal ulceration, corneal perforation, and blindness. Cryopreserved amniotic membrane contains anti-inflammatory mediators, a myriad of growth factors and cytokines, and a regenerative matrix that is important to help restore a healthy and noninflamed ocular surface and maintain a stable tear film.
Diagnosis
- Symptoms: Ocular irritation, burning, itching, pain, foreign-body sensation, photophobia, and blurred vision
- Examination: Conjunctival injection/inflammation, decreased tear meniscus, decreased tear break-up time, increased debris in the tear film/mucous discharge, corneal filaments, irregular corneal surface, superficial punctate keratitis (SPK) with positive fluorescein staining, and corneal ulcers/infectious keratitis in severe cases
Treatment Strategy
- Administer artificial tears, preferably nonpreserved
- Treat ocular surface inflammation with steroid or RESTASIS®
- Perform punctal occlusion with plug or cautery
- Restore corneal integrity by suppressing inflammation and restoring a healthy, normal epithelium (PROKERA®)
Case Study
- A 49-year-old female presented with persistent ocular discomfort, gritty sensation, and blurred vision (20/100) for 1 week. She had a long history of dry eye and rheumatoid arthritis and has been treated with artificial tears, serum eye drops, punctal plugs, and a scleral lens without success.
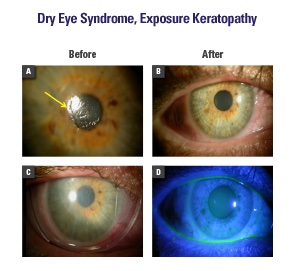
- Examination showed an irregular corneal epithelium with SPK (Fig. A)
- PROKERA® was placed (Fig. C) to restore a smooth epithelium within 48 hours, resulting in complete symptomatic relief, clear cornea, and 20/20 vision (Fig. B, D)
Conclusion
PROKERA® can be used as a temporary biological bandage for severe DES to restore a healthy and smooth corneal epithelium and reduce inflammation that is crucial in maintaining a stable tear film.
