Filamentary Keratitis
Filamentary Keratitis
Highland Ophthalmology
Mary Davidian, MD, is a cornea specialist and medical director at Highland Ophthalmology Associates in New Windsor, NY. DR. Davidian completed her residency at the New York Eye and Ear Infirmary and a cornea fellowship at UC Irvine. She is an active participant of multiple ophthalmology societies. She is a consultant and speaker for BIO‑TISSUE® and can be reached at (845) 562-0138.

MARY DAVIDIAN, MD – NEW WINDSOR, NY
Overview
Filamentary keratitis is a chronic corneal condition characterized by multiple filaments attached to areas of compromised corneal epithelium. The filaments can be quite extensive and may enmesh calcareous granules, bacteria, and dust particles. Blinking lids pull on the loose ends of the filaments, stimulating the pain-sensitive corneal nerves and creating multiple epithelial defects. Patients often experience foreign body sensation, discomfort, photophobia, pain, and blurry vision. Filamentary keratitis most often accompanies dry eye syndrome and patients may also have underlying systemic conditions, particularly connective tissue disorders. Cryopreserved amniotic membrane contains anti-inflammatory mediators and complex arrays of growth factors and cytokines, which help regenerate a healthy corneal epithelium and may reduce recurrence.
Diagnosis
- Symptoms: Ocular discomfort, foreign body sensation, pain, photophobia, and blurred vision.
- Examination:
Tadpole-shaped mucus filaments adhering to the corneal surface, with the tails floating freely within the tear film - Rose bengal dye makes the filaments more readily visible on biomicroscopy
- Reduced tear break-up time and punctate epithelial keratopathy
Treatment Strategy
- Treat ocular surface inflammation (nonpreserved steroids)
- Treat associated dry eye (artificial tears/punctal occlusion)
- Restore corneal integrity (PROKERA®)
- Prophylactic antibiotics if necessary
Case Study
- A 68-year-old female presented with acute ocular pain, photophobia, and blurred vision (20/70) for 3 days. She had a history of similar repeated attacks as well as dry eye (treated with artificial tears and punctal plugs).
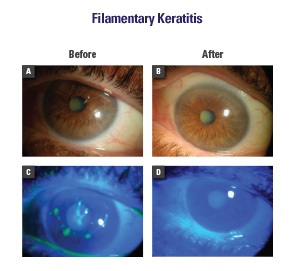
- Diagnosis of filamentary keratitis was confirmed based on the clinical findings of positively stained mucus strands attached to the cornea (Fig. A, C)
- Numerous treatment regimens were implemented, including non-preserved artificial tears, lubricating ointment, and topical steroids for 2 months without success
- Without debridement, PROKERA® was placed for 3 days. Her symptoms were completely relieved, filaments disappeared, and the cornea became clear (Fig. B, D). Her vision improved to 20/40.
Conclusion
Filamentary keratitis is a recurrent and incapacitating condition that may prove difficult to manage. PROKERA® effectively treated the above patient and restored a healthy corneal epithelium.
