Infectious Keratitis
Highland Ophthalmology
Mary Davidian, MD, is a cornea specialist and medical director at Highland Ophthalmology Associates in New Windsor, NY. DR. Davidian completed her residency at the New York Eye and Ear Infirmary and a cornea fellowship at UC Irvine. She is an active participant of multiple ophthalmology societies. She is a consultant and speaker for BIO‑TISSUE® and can be reached at (845) 562-0138.

MARY DAVIDIAN, MD – NEW WINDSOR, NY
Overview
Infectious keratitis is a serious sight-threatening ocular infection and one of the most significant complications of contact lens usage. Damage to the cornea can occur rapidly and early diagnosis and treatment are essential. The principal therapeutic goal is to eliminate the pathogens and to prevent irreversible corneal structural damage. After the pathogen is identified by microbiological workup, topical antimicrobial therapies take precedence to sterilize the corneal lesion. Despite the control of infection, corneal melting/damage/scarring may occur due to digestive enzymes released by inflammatory and immune reactions to microbes. Cryopreserved amniotic membrane is well known to have potent anti-inflammatory and anti-scarring properties that promote healing and prevent corneal melt and scar formation. In addition, due to its therapeutic effects, cryopreserved amniotic membrane may also facilitate reduced steroid usage.
Diagnosis
- History: Injury, contact lens usage, or surgery
- Symptoms: Pain, photophobia, lacrimation, and loss of vision
- Examination: Corneal epithelial defect with infiltrate or ulcer, corneal edema, and hypopyon
Treatment Strategy
- Perform scraping and microbial culture
- Treat infection with fortified broad-spectrum antibiotics, which will be modified according to culture results
- Treat the inflammation and prevent corneal melting (PROKERA®)
- Restore corneal integrity by promoting healing and reducing haze (PROKERA®)
Case Study
- A 61-year-old LASIK and contact lens wearer presented with severe ocular pain and loss of vision
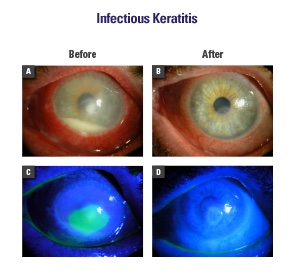
- Examination revealed a central corneal ulcer, deep stromal infiltrate, hypopyon, and severe conjunctival inflammation (Fig. A, C)
- Corneal scraping and culture were followed by fortified antibiotics. Microbiologic workup confirmed the diagnosis of staphylococcus aureus.
- PROKERA® was placed and fortified antibiotics were tapered to QID
- Two weeks later, inflammation was markedly reduced, the corneal epithelial defect completely healed, and the patient regained 20/25 vision (Fig. B, D)
Conclusion
Early intervention by PROKERA® promotes epithelialization and reduces pain, inflammation, and haze in severe bacterial keratitis.
