Post-DSEK for Bullous Keratopathy
Post-DSEK for Bullous Keratopathy
Eye Institute of West Florida
Neel R. Desai, MD, is a fellowship-trained ophthalmologist strictly specializing in LASIK, cataract and corneal diseases of the eye. Dr. Desai is a top graduate of the Pennsylvania State University College of Medicine and completed his fellowship in cornea, cataract, and refractive surgery at the Wilmer Eye Institute at Johns Hopkins University. Dr. Desai is in private practice at the Eye Institute of West Florida with offices in Largo, Clearwater, and St. Petersburg, Florida. He is a consultant and speaker for BIO-TISSUE® and can be reached at (727) 581-8706.

NEEL DESAI, MD – LARGO, FL
Overview
Descemet’s stripping endothelial keratoplasty (DSEK) is currently the treatment of choice over penetrating keratoplasty in cases with bullous keratopathy due to corneal endothelial dysfunction. Advantages include faster recovery and fewer complications. In cases with pseudophakic bullous keratopathy (PBK), the stromal and epithelial edema usually interferes with intraoperative visualization and poses a major technical challenge for DSEK. Debridement of the epithelial blisters may improve the visualization during surgery; however, it creates a large, slow-healing epithelial defect.
Cryopreserved amniotic membrane has been used successfully to treat nonhealing epithelial defects. Early intervention with cryopreserved amniotic membrane via PROKERA® enhances faster healing of a large corneal epithelial defect after DSEK in a case of PBK.
Diagnosis
- Symptoms: Ocular pain, foreign-body sensation, photophobia, and loss of vision
- Examination: Corneal opacity, edema, vascularization, and epithelial bullae/defects
Treatment Strategy
- DSEK to replace diseased endothelium
- Debridement/superficial keratectomy to remove diseased epithelium and
improve visualization during DSEK - PROKERA® placement to enhance epithelialization and reduce haze
Case Study
- An 85-year-old patient presented with light perception vision and persistent pain in the right eye following cataract surgery
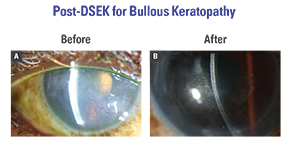
- Examination revealed PBK with large corneal epithelial bullae, corneal haze, vascularization, and edema (Fig. A)
- Superficial keratectomy was performed to remove the corneal pannus and to improve visualization. DSEK was then performed through a temporal 4-mm scleral tunnel. PROKERA® was placed to enhance epithelialization.
- The corneal epithelium completely healed in 1 week. The superficial and deep corneal neovascularization regressed and completely vanished after 1 month. The posterior lamellar graft remained stable, and vision improved to 20/70 at 2 months, 20/50 at 2 years and 20/40 at 3 years (Fig. B).
Conclusion
PROKERA® can be used as a temporary biological bandage to restore a healthy corneal epithelium after dseK is used to restore a functioning corneal endothelium.
