Eye Institute of West Florida
Neel R. Desai, MD, is a fellowship-trained ophthalmologist strictly specializing in LASIK, cataract and corneal diseases of the eye. Dr. Desai is a top graduate of the Pennsylvania State University College of Medicine and completed his fellowship in cornea, cataract, and refractive surgery at the Wilmer Eye Institute at Johns Hopkins University. Dr. Desai is in private practice at the Eye Institute of West Florida with offices in Largo, Clearwater, and St. Petersburg, Florida. He is a consultant and speaker for BIO‑TISSUE® and can be reached at (727) 581-8706.

NEEL DESAI, MD – LARGO, FL
Overview
Salzmann’s Nodular Degeneration (SND) is characterized by multiple superficial blue-white nodules in the midperiphery of the cornea. The pathogenesis is unknown and usually develops following ocular surface inflammation or surgery as an end-stage of the corneal scarring pathway. SND is usually asymptomatic but may affect vision if located centrally. Histologically, SND is composed of dense irregularly arranged collagen tissue between epithelium and Bowman’s layer or beyond; therefore, patients may develop recurrent corneal erosions or corneal scarring.
Surgical removal, phototherapeutic keratectomy (PTK) with or without the use of topical mitomycin C (MMC), lamellar, or penetrating keratoplasty have been used in the treatment of this disease. Although PTK may restore a smooth ocular surface, the required laser ablation depth is significantly large and may be complicated with haze and refractive error. In contrast, superficial keratectomy followed by placement of PROKERA® is effective in restoring corneal surface integrity without haze.
Diagnosis
- History: Previous inflammation, corneal surgery
- Symptoms: Decreased vision if located centrally
- Examination: Superficial, elevated multiple blue-white nodules located at corneal midperiphery
Treatment Strategy
- Removal of corneal lesion (superficial keratectomy)
- Restoring corneal surface integrity by promoting healing and preventing haze (PROKERA®)
Case Study
- A 36-year-old male presented with progressive distortion of vision in both eyes 20 years after radial keratectomy
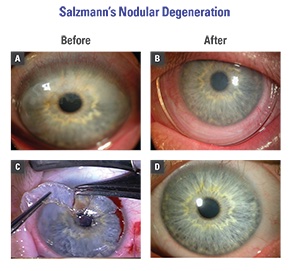
- SND encroaches on the visual axis resulting in 20/70 vision (Fig. A)
- Superficial keratectomy was performed (Fig. C), followed by topical MMC for 25 seconds and placement of PROKERA®
- Complete epithelialization was achieved without haze in 6 days (Fig. B)
- The cornea was clear 3 weeks later and vision improved to 20/20 (Fig. D). No recurrence was noted during a 2-year follow-up.
Conclusion
PROKERA® allows regenerative healing to restore corneal surface integrity and improve the quality of vision after superficial keratectomy to remove Salzmann’s nodular degeneration or other similar diseases.
