
Urology Awareness Month
Prolonged inflammation can impact Urology patients’ outcomes.
Clarix® is the answer.
Clarix 1K is a cryopreserved ultra-thick human birth tissue allograft used as an adjunct for surgical applications. Clarix 1K helps support a regenerative healing environment and the restoration of urinary and sexual function after Robot-Assisted Radical Prostatectomy (RARP). 1-2

Maximizing Patient Care Matters.
At the time of surgery, provide an opportunity for improved clinical outcomes with Clarix.
Images courtesy of Mutahar Ahmed, MD, Hackensack Meridian Health, Hackensack, NJ
The Proof is in the Evidence
Improved clinical outcomes are supported by our published clinical evidence in Urologic Oncology applications:
83% of patients achieved continence at 3-months when Clarix was used as an adjunct in RARP.1
75% of patients achieved potency at 6-months post-RARP with the use of Clarix.2
Clarix is an ultra-thick allograft providing ease of use in robotic procedures.
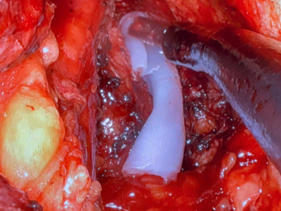
Allograft placement over Neurovascular Bundles (NVBs) after prostate resection.

Introducing allograft into the surgical site using a single-port robot.



