Recurrent Corneal Erosion
Recurrent Corneal Erosion
Ophthalmic Consultants of Chicago
Robert Mack, MD, is a magna cum laude graduate of Cornell University and graduated with distinction from Case Western Reserve University School of Medicine, where he served as president of the medical honor society. Dr. Mack is the recipient of both the Arthur J. Maschke Award for Excellence in the Art and Science of Medicine and the Irwin H. Lepow Award for Excellence in Research. He is a board-certified ophthalmologist with complete fellowship training in corneal and refractive surgery. Dr. Mack has served as an Assistant Professor of ophthalmology at rush Medical college and as co-investigator on several excimer laser clinical trials. He is also a member of the editorial board of the Journal of Refractive Surgery. He is not a consultant for BIO‑TISSUE®.
ROBERT MACK, MD – CHICAGO, IL
Overview
Recurrent corneal erosion (RCE) is a common ocular disorder characterized by a disturbance at the level of the corneal epithelial basement membrane (BM), resulting in defective adhesions and recurrent breakdown of the epithelium.8 RCE may occur spontaneously or secondary to corneal injury. Predisposing factors include diabetes or corneal dystrophy.9 Patients with RCE often show increased levels of enzymes such as matrix metalloproteinases (MMPs) that dissolve the BM and its anchoring components including integrins, laminin, and type VII collagen.10
Noncryopreserved treatments include lubricating agents, patching, bandage contact lenses (BCLs), debridement, anterior stroma puncture, and phototherapeutic keratectomy (PTK). However, these treatments still have a high recurrence rate and carry the risk of developing haze.8 Cryopreserved amniotic membrane contains inhibitors of MMPs and active matrix components including collagen type VII and laminin, essential for regenerative healing and prevention of recurrence.11
Diagnosis
- History: Previous corneal injury, corneal dystrophy, or diabetes
- Symptoms: Acute ocular pain, foreign-body sensation, photophobia, and tearing (upon awakening)
- Examination: Punctate epithelial erosions in milder cases (microform erosions) and a large epithelial defect or area of edematous nonadherent epithelium in severe cases (macroform erosion)
Treatment Strategy
- Relieve acute symptoms (eg, pain)
- Restore corneal integrity, regain epithelial attachments, and prevent recurrence (PROKERA®)
- Treat underlying cause
- Reduce the risk of secondary infections (avoid extended BCL usage)4
Case Study
- A 52-year-old female presented with ocular pain and blurred vision (20/200) for 2 weeks
- She had a history of similar attacks diagnosed as RCE. Epithelial debridement, lubricants, and BCLs failed to relieve pain and halt recurrence.
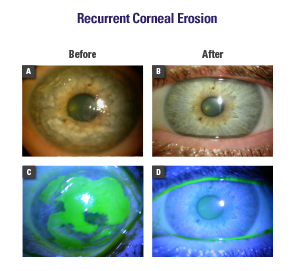
- Epithelial debridement to remove loose epithelium (Fig. A, C) followed by placement of PROKERA® (Fig. B)
- On the second day, the patient had no pain
- Complete healing occurred within 3 days, resulting in a clear cornea and 20/20 vision (Fig. D)
- Cornea remained stable with no recurrence for more than 2 years of follow-up
Conclusion
PROKERA® rapidly resolved RCE and prevented further recurrence in this case, which failed to respond to conventional therapies.
